
World Cancer Day, observed annually on 4 February, is a global moment for reflection, awareness, and action. The 2025–2027 theme, “United by Unique,” calls for a fundamental shift in how the world understands and delivers cancer care: from systems built around diseases to systems designed around people. This article explores the meaning behind the theme, why a people‑centered model matters, and how individuals, communities, and institutions can work together to build a future in which every person’s story guides care. By recognizing that every experience of cancer is unique—and by uniting across sectors and societies—we can create a world that looks beyond the disease and truly sees the person.1,2,3
Every year on 4 February, World Cancer Day brings together patients, survivors, caregivers, clinicians, researchers, policymakers, and advocates in a shared purpose: to raise awareness, reduce stigma, promote equitable access to care, and inspire tangible improvements in prevention, diagnosis, treatment, and survivorship. But beyond the statistics and strategies lies a deeper human truth—cancer is never just a medical condition. It touches identity, family, livelihood, hopes, and community.4
The theme for 2025–2027, “United by Unique”, puts this truth at the center. It reminds us that while cancer is a global challenge, its impact is deeply individual. Two people with the same diagnosis will not have the same journey. Different cultures, ages, languages, genders, incomes, and life circumstances shape how cancer is understood, experienced, and treated. Recognizing and honoring this individuality is not a “nice‑to‑have”—it is essential to achieving the best outcomes and sustaining dignity at every step of care.5
The burden of cancer continues to grow, and so do disparities. People in different regions, income groups, and communities often face unequal access to prevention, early detection, modern therapies, and supportive care. Some face social stigma or legal barriers; others navigate fragmented systems or unaffordable costs. In this context, people‑centered, equity‑driven approaches are critical.6,7
Embracing the theme means:7-12
• Improving early detection through culturally appropriate outreach and education, delivered in the languages and channels people trust.
• Reducing financial toxicity by expanding coverage, transparent pricing, patient navigation, and employer policies that protect income and jobs.
• Integrating mental health into routine care, recognizing anxiety, depression, trauma, and caregiver stress as core clinical concerns.
• Leveraging technology thoughtfully, ensuring telehealth and digital tools connect, not exclude, people with limited connectivity or digital literacy.
• Championing palliative care as a right, not a last resort—available early, alongside curative or life‑prolonging treatments.
• Focusing on survivorship: rehabilitation, return‑to‑work programs, fertility and sexual health services, and long‑term follow‑up for late effects.
In short, centering people leads to better engagement, better adherence, better outcomes—and a more humane system for all.
Traditional cancer systems tend to be organized around diagnoses, protocols, and facilities—important foundations that enable consistent, evidence‑based care. Yet these structures can inadvertently marginalize the personal, social, and cultural factors that determine whether care is accessible, acceptable, and effective for each person. A people‑centered approach rebalances that equation. It integrates the science of medicine with the art of listening, empathy, and co‑design.13
A people‑centered cancer system:7-9,13-15
• Sees the whole person, not just the tumor: their values, beliefs, family roles, work obligations, and goals for care.
• Plans with, not for the patient: shared decision‑making that respects autonomy and preferences.
• Coordinates across the continuum: prevention, screening, diagnosis, treatment, rehabilitation, palliative care, and survivorship support are linked and navigable.
• Respects diversity: care is culturally sensitive and linguistically appropriate; it addresses gender, age, disability, and socio‑economic contexts.
• Builds trust and compassion: communication is clear, honest, and supportive; mental health and social support are embedded, not optional.
• Focuses on equity: addresses barriers like distance, cost, stigma, legal status, and digital divides that prevent people from getting timely help.
This is not a rejection of medical excellence. It is an expansion of it—where compassion, lived experience, and clinical expertise reinforce each other.
Turning principle into practice requires both mindset shifts and practical tools. Here is a patient-centered communication framework organizations can adopt (Figure 1): The six core functions of patient-clinician communication overlap and interact to produce communication that can affect important health outcomes.
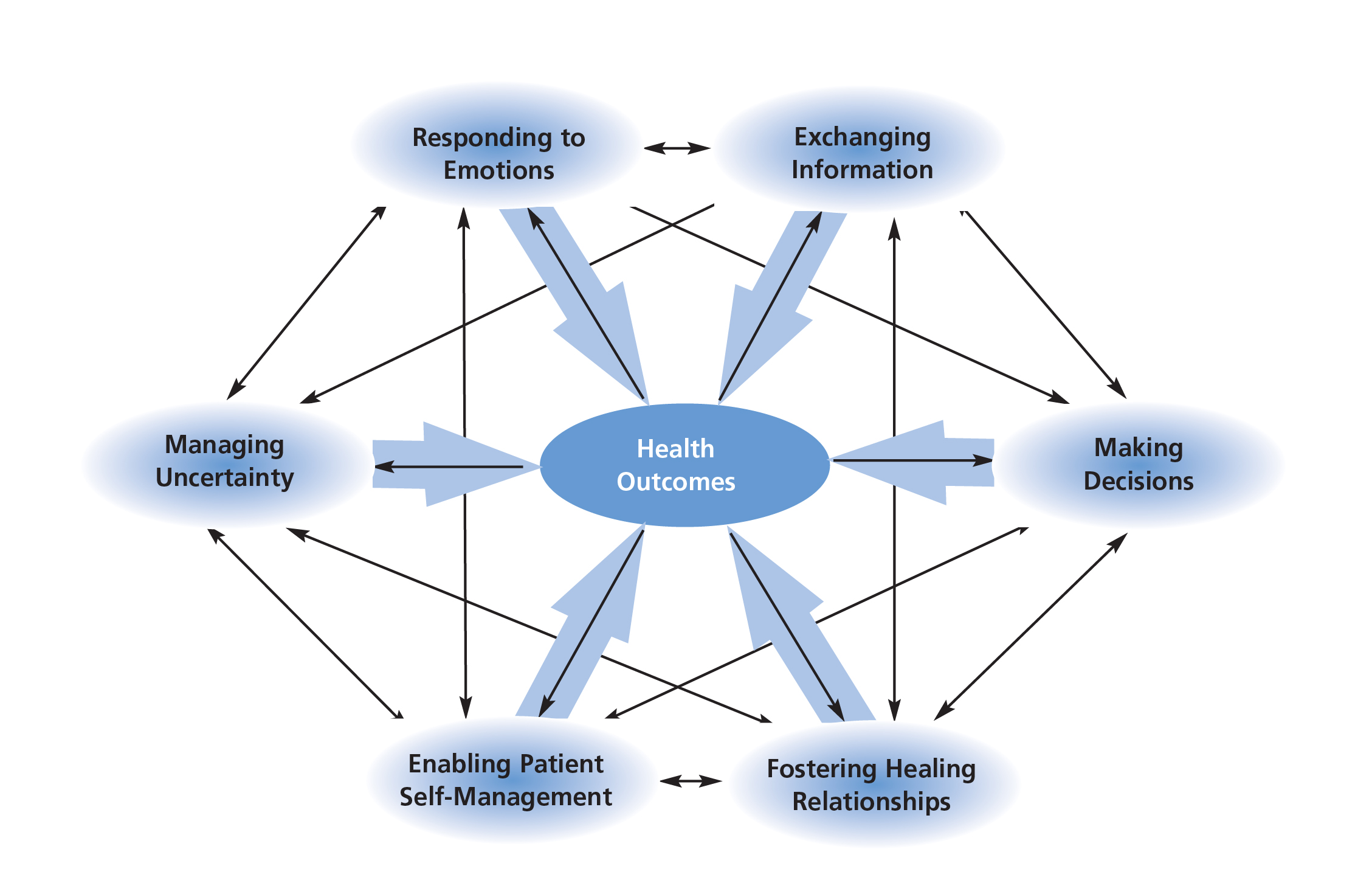
Figure 1: National Cancer Institute framework for patient-centered communication16
• Exchanging information emphasizes the importance of recognizing patients’ information needs, integrating clinical information with the patient’s illness representations, acknowledging both the content and process of information exchange, recognizing that disease-related information now is more available through the Internet, communicating prognostic information accurately while also providing hope, and overcoming barriers related to low health literacy and poor understanding of statistical information.
• Responding to emotions requires clinicians to elicit patients’ emotional distress; communicate an understanding of the patient’s emotions to him or her; and respond with legitimation, validation, empathy, and support.
• Managing uncertainty emphasizes that uncertainty often cannot be eliminated but can be managed by providing information, support, and cognitive strategies to help patients and families deal more effectively with the anxiety related to uncertainty.
• Making decisions involves consideration of both the active involvement of the patient and family in the information exchange and deliberation stages of the decision-making process and the identification of the person responsible for the final decision.
• Lastly, enabling patient self-management involves advocacy for the patient, including navigating the patient through the health care system; supporting patient autonomy; and providing guidance, skills, and access to resources.
Creating people‑centered cancer care is a shared responsibility. Healthcare professionals can champion empathetic communication, inter‑disciplinary teamwork, and personalized plans. Healthcare organizations can resource navigation services, embed mental health, and measure what matters to patients. Policymakers can expand coverage, protect employment rights, and fund community‑based prevention and early detection. Employers can offer flexible leave, accommodations, and stigma‑free return‑to‑work policies. Researchers and innovators can include diverse populations in trials and co‑design tools with end users. Educators and media can reduce stigma and spread accurate, accessible information. Communities and faith‑based groups can provide practical support, connection, and trust.
Additionally, individuals—with or without a direct link to cancer—can contribute by learning, listening, donating, volunteering, advocating, and checking in on neighbors and colleagues. Small acts add up. When we look beyond the disease and truly see the person, care becomes not only more compassionate—it becomes more effective.1
Stories humanize data. Behind every diagnosis is a life story. Some are stories of grief, as individuals and families face uncertainty or loss. Others are stories of pain, both physical and emotional, that require skill and sensitivity to manage. Many are stories of healing and resilience, charting pathways through treatment, adaptation, and newfound strengths. Furthermore, numerous stories are rooted in love—communities rallying, caregivers holding steady, friends showing up, workplaces accommodating, and health professionals offering care beyond the call of duty.
On this World Cancer Day, consider whose story you can uplift: a survivor’s return to joy, a caregiver’s quiet strength, a clinician’s steadfast presence, or a community’s collective response. Stories connect us—united by what is unique in each person.
As World Cancer Day 2026 approaches, “United by Unique” invites us to transform how we think about and deliver cancer care. It asks us to place people at the center, to recognize that behind every diagnosis is a singular story that deserves respect, empathy, and partnership. A people‑centered approach is not an optional enhancement; it is the pathway to better outcomes, greater equity, and dignified care. When we unite—patients and survivors, families and clinicians, employers and policymakers, researchers and advocates—we create systems that look beyond the disease and truly see the person. In doing so, we honor every story and move closer to a world where compassionate, personalized, and equitable cancer care is a reality for all.
United by our shared humanity, strengthened by our unique journeys—this is how we change the future of cancer care.
References
1. Elkefi S and Asan O. J Patient Exp. 2023;10:23743735231151533. 2. McCormack LA, et al. Soc Sci Med. 2011;72(7):1085-95. 3. Goodwin N. Int J Integr Care. 2014;14:e026. 4. Craig S, et al. Healthcare (Basel). 2023;11(24):3166. 5. NHS England. Personalised care and improving quality of life outcomes. Available from: https://www.england.nhs.uk/cancer/living/. [Accessed 15 January 2026]. 6. Hussaini SMQ, et al. JCO Oncol Pract . 2025 Nov 14:OP2500946. doi: 10.1200/OP-25-00946. Online ahead of print. 7. Oyer RA, et al. JCO Oncol Pract. 2021;17(5):215-8. 8. Rost M, et al. Eur J Oncol Nurs. 2023;64:102277. 9. Caruso R and Breitbart W. Epidemiol Psychiatr Sci. 2020;29:e86. 10. Jain S, et al. J Healthc Leadersh. 2024;16:525-35. 11. Howie L and Peppercorn J. Ther Adv Med Oncol. 2013;5(6):318-23. 12. Neuman HB and Schumacher JR. Surg Clin North Am. 2023;103(1):169-85. 13. Yang Y, et al. Health Expect. 2020;23(2):274-83. 14. Shickh S, et al. Am Soc Clin Oncol Educ Book. 2023;43:e389516. 15. Vos JAM, et al. EClinicalMedicine. 2025;90:103599. 16. Epstein RM and Street RL Jr. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. National Cancer Institute, NIH Publication No. 07-6225. Bethesda, MD, 2007.





