The Autonomous Sensory Meridian Response (ASMR) is a pleasant tingling sensation, typically beginning on the scalp and spreading down the neck and spine, and is elicited by a range of specific auditory, visual, or tactile stimuli, such as whispering, tapping, or gentle hand movements1. Although existing literature suggests that ASMR triggers differ among individuals, watching ASMR videos has become a popular way to relax and alleviate symptoms of stress and insomnia2. Accordingly, the therapeutic potential of ASMR has attracted the interest of researchers and clinicians. Nonetheless, the underlying physiological mechanism of ASMR is still not fully understood. The purpose of this article is to review published literature on the physiology of ASMR and discuss its therapeutic potential in various psychiatric conditions.
ASMR occurs involuntarily and is induced by focusing on auditory, tactile, or visual triggers, such as watching someone else hair brushing or listening to whispers or tapping2. Before being known as ASMR, this tingling sensation of wellbeing and intense relaxation was referred to as "brain orgasm", though the phenomenon is widely described as non-sexual. Unlike most physiological phenomena, the first reported discussion of ASMR was on an informal internet health forum in 2007, whereas the term ASMR was subsequently coined by Jennifer Allen in 20103. Since then, ASMR has gained popularity globally on the internet. For instance, there are currently millions of ASMR videos on YouTube, and many ASMR videos have attracted an enormous number of views, while one of them has reached over 46 million views4.
Although ASMR has blossomed into an international phenomenon, its effectiveness in inducing relaxation is inconsistent. This can be partly explained by the ambiguous definition of ASMR and the subjective outcome measures leading to difficulties in distinguishing between ASMR and similar sensations, such as frisson or synaesthesia5.
Notably, a study by Barratt et al. (2017) involving 130 people who self-reported experiencing ASMR revealed that the induction of ASMR can be influenced by various aspects of the triggers, including timing and trigger load, atmosphere, characteristics of ASMR content, etc6. Moreover, a survey by Poerio et al. (2022), which recruited 648 working adults and students, indicated that the proportion of ASMR responders among those who reported watching ASMR content was 62.6 (Figure 1)5. Therefore, ASMR appears to be a highly personal and wide-ranging event.
-5.jpg)
Figure 1: Proportion of SMR responders among those who reported watching ASMR content5
In order to address the objective descriptions of ASMR outcomes, emerging studies investigate the physiological changes associated with ASMR. For instance, the study by Engelbregt et al. (2022) involving 38 adults aged 17-35 years exposed to ASMR video evaluated the changes in heart rate (HR) and skin conductance associated with ASMR. In the study, 15 participants out of 38 were classified as ASMR-experiencers according to the responses to the questions of the ASMR-checklist7.
Essentially, the results indicated that a decrease in HR during watching the ASMR video was detected in all participants, irrespective of experiencing tingles. Remarkably, in ASMR-experiencers with low conscientiousness electrodermal activity (EDA) exhibited a significant increase in average EDA under the ASMR condition than the control condition in the tingles group, while no significant change was seen in the no tingles group (p = 0.077, Figure 2)7.
 on mood, attention, heart rate, skin conductance and EEG in healthy young adults-9.jpg)
Figure 2: Mean skin conductance in the Tingles and No-tingles group within the ‘low conscientiousness’ group7
As reflected in electroencephalography (EEG) recordings, watching ASMR video was associated with a decreased alpha power in ASMR-sensitive participants, and a decreased theta as well as increased beta power in the whole group of participants7. Thus, the observed ASMR-induced changes in EEG and EDA suggested that ASMR is related to arousal and focused attention.
Interestingly, Lochte et al. (2018) illustrated the brain activation when watching ASMR videos and identified specific moments of relaxation and tingling using functional magnetic resonance imaging (fMRI)-based methodology. The study showed that the subjects who experienced ASMR (n=10) showed significant activation in regions associated with both reward (nucleus accumbens [NAcc]) and emotional arousal (dorsal anterior cingulate cortex [dACC] and insula/inferior frontal gyrus [IFG], Figure 3A and 3B). The report suggested that brain activation during ASMR showed similarities to patterns previously observed in musical frisson and affiliative behaviours8.
-6.jpg)
Figure 3: Whole brain activation during A) relaxing moments and B) tingling moments when contrasted with baseline moments8
More recently, Sakurai et al. (2023) compared the differences between auditory and audiovisual stimulation in terms of the areas of activation in the brain upon exposure to ASMR videos with fMRI. In particular, this study identified the specific sites of activation for audiovisual stimulation, which were the middle frontal gyrus (MFG) and the left NAcc (Figure 4), and the specific sites of activation for auditory stimulation, which were the bilateral insular cortices9.
 video viewing-5.png)
Figure 4: WActivation during the ASMR audiovisual stimulation task showing A) activation of the left NAcc and B) activation of the left MFG9
Although the physiological basis of ASMR is yet to be fully understood, its practical benefits have attracted research interest, and numerous studies have been conducted to evaluate the efficacy of ASMR in improving wellbeing. For instance, as per the study by Engelbregt forementioned, depressive feelings significantly decreased after watching the ASMR video in individuals experiencing tingles than those not experiencing tingles7.
More recently, Kim and Park (2024) investigated the effects of breathing-relaxation training plus ASMR on mood and depressive symptoms in patients with mild depression. In the study, 40 patients were assigned to the experimental group that received breathing-relaxation training plus ASMR or the wait-list control group for a total of 8 training sessions. The results indicated that the experimental group achieved a significantly greater improvement in mood and depressive symptoms with more ASMR experiences (19.30±2.25 [pre-test depression score] vs 7.75±1.20 [post-test depression score]) compared to the control group (15.20±1.47 [pre-test depression score] vs 15.70±1.26 [post-test depression score], p<0.001)10.
Apart from depression, the investigation by Eid et al. (2022), which recruited 36 ASMR experiencers and 28 non-experiencers, demonstrated that exposure to ASMR video significantly attenuated pre-video state anxiety (41.75 [pre-ASMR video] vs 36.58 [post-ASMR video]). Of note, there was no difference in state anxiety pre- and post-video reported among non-experiencers (35.04 [pre-ASMR video] vs 35.14 [post-ASMR video], Figure 5)2. Accordingly, watching ASMR appeared to alleviate state anxiety but only in those who experienced ASMR.
, neuroticism, and trait & state anxiety-8.jpg) Figure 5: Mean state anxiety scores of ASMR-experiencers and non-experiencers2
Figure 5: Mean state anxiety scores of ASMR-experiencers and non-experiencers2
While ASMR is widely reported to be accompanied by feelings of relaxation and wellbeing, it is widely used as a sleep aid. A survey involving 475 participants by Barratt and Davis (2015) revealed that 82% of participants agreed that they used ASMR to help them sleep. Hence, 81% of participants reported that the time before sleeping at night was their preferred time for engagement with ASMR media. Interestingly, the survey further reported that sleeping pills dulled the participants' ASMR experience4.
Subsequently, Lee et al. (2019) tried to induce sleep with a 6 Hz binaural beat combined with ASMR. The binaural beat corresponding to the centre of the theta band (4–8 Hz), which is the frequency at which brain activity is entrained during non-rapid eye movement (NREM) in sleep stage 1. In addition, ASMR presented from natural sound was included to exploit the feelings of calmness and relaxation. As confirmed with EEG data analysis, the combination of a 30:60 dB ratio of binaural beat to ASMR trigger is most effective for inducing the brain signals required for sleep, while simultaneously keeping the user in a psychologically comfortable state11. Nonetheless, clinical trials confirming the effectiveness of ASMR in improving sleep quality are preferred.
Existing literature suggested that ASMR may be applied to alter the brain states, which in turn helps control chronic conditions, such as pain syndromes6. Recall the audiovisual stimulation of the MFG and NAcc by ASMR reported in Sakurai's study above, the stimulation plays an important role in the mesolimbic dopamine pathway, which operates as a reward mechanism. Particularly, NAcc is an important brain region for reward, gratification, and emotion and is largely responsible for the release of dopamine. It is involved in improving pain, depression, and anxiety symptoms as well9.
Recent research by McErlean et al. (2022) evaluated the link between sensory sensitivity and ASMR. In the study, ASMR experiencers and controls were recruited to administer an algometer and a visual analogue scale (VAS) to measure the pain sensitivity following an ASMR video and a control video. Findings indicate that ASMR experiencers had a higher pain sensitivity than controls. However, there was no difference between the two groups in terms of pain tolerance. The report concluded that any potential analgesic properties associated with experiencing ASMR may reflect protective properties of ASMR buffering against the increased pain sensitivity among ASMR experiencers relative to controls12.
As per existing literature, ASMR is generally a safe method for stress reduction. Nonetheless, a previous survey by McErlean and Banissy (2018) reported that individuals exposed to ASMR (n = 64) scored higher than controls (n = 68) on all subscales of Misophonia Questionnaire (MQ), including the Misophonia Symptom Scale, the Misophonia Emotions and Behaviours Scale and the Misophonia Severity Scale (Figure 6)13. The findings suggested that individuals with ASMR experience may have elevated levels of misophonia. Thus, personalising trigger selection is crucial in applying ASMR.
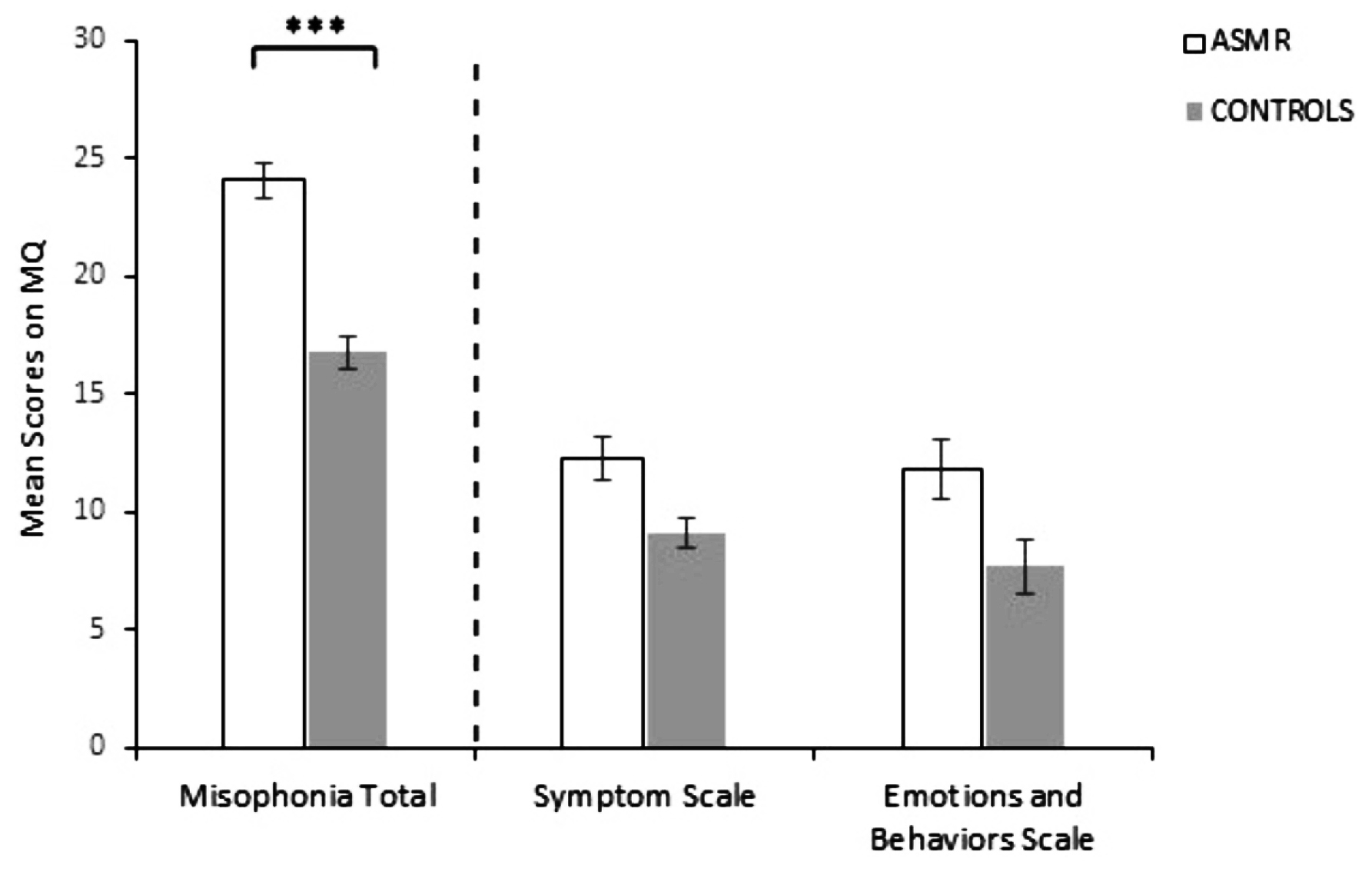 Figure 6: Mean responses for ASMR-responders and controls on the MQ13, ***p<0.001
Figure 6: Mean responses for ASMR-responders and controls on the MQ13, ***p<0.001
Another issue concerning ASMR is the lack of solid evidence supporting its efficacy. Notably, most existing findings of ASMR relied on self-reporting data, whereas reports with objective outcome measures are inadequate. This limits the validity of findings and raises questions about the role of placebo effect in ASMR’s perceived benefits.
The promising findings of ASMR have highlighted its potential roles in managing various clinical conditions. Essentially, ASMR could be integrated into clinical settings as a low-cost, non-invasive intervention for anxiety and insomnia. For example, tailored ASMR protocols could be developed for cognitive-behavioural therapy (CBT) or mindfulness-based interventions. Of course, further studies improving our understanding of the physiological basis of ASMR and identifying its biomarkers, possibly utilising advances in neuroimaging techniques, are highly desirable to optimise and individualise ASMR.
References
1. Poerio et al. PLoS One 2018; 13. DOI:10.1371/JOURNAL.PONE.0196645. 2. Eid et al. PLoS One 2022; 17: e0262668. 3. Trenholm-Jensen et al. PLoS One 2022; 17: e0277962. 4. Barratt et al. PeerJ 2015; 2015: e851. 5. Poerio et al. Front Psychol 2022; 13: 990565. 6. Barratt et al. PeerJ 2017; 2017: e3846. 7. Engelbregt et al. Exp Brain Res 2022; 240: 1727. 8. Lochte et al. Bioimpacts 2018; 8: 295. 9. Sakurai et al. Front Neurosci 2023; 17: 1025745. 10. Kim et al. Psychiatry Investig 2024; 21: 1102–9. 11. Lee et al. Front Hum Neurosci 2019; 13: 425. 12. McErlean et al. Perception 2022; 51: 565–77. 13. McErlean et al. PeerJ 2018; 2018: e5351.





