
Chronic insomnia is a widespread condition among middle-aged and older adults, yet access to first-line treatment¡XCognitive Behavioral Therapy for Insomnia (CBT-I)¡Xremains limited due to cost and therapist availability. This article examines findings from a large randomized non-inferiority trial comparing Tai Chi, a traditional mind¡Vbody practice, with CBT-I in adults aged 50 and above. While Tai Chi was less effective than CBT-I immediately after the three-month intervention, it achieved non-inferior long-term improvements at the 12-month follow-up. Both groups demonstrated significant enhancements in insomnia severity, sleep quality, mental wellbeing, and physical functioning, with no adverse events reported. The results highlight Tai Chi as an accessible, low-cost, and sustainable alternative for long-term management of chronic insomnia in aging populations.1
Chronic insomnia is one of the most prevalent sleep disorders among middle-aged and older adults, affecting up to 50% of individuals in Hong Kong and between 4% to 22% globally.2,3 Beyond the nightly struggle to fall asleep, insomnia carries severe consequences¡Xheightened risks of cardiovascular disease, mental health disorders, cognitive decline, and even increased mortality.4 The economic toll is staggering, with annual costs in the United States alone estimated at $150 billion.5
The first line treatment for insomnia is CBT-I, praised for its efficacy and minimal side effects.6 Yet, CBT-I faces barriers: high costs, limited availability of trained therapists, and low referral rates.7,8 Data from 12 European countries indicate that only 4-10% of patients are prescribed nonpharmacological insomnia treatments such as CBT-I.9 This accessibility gap has sparked interest in alternative, cost-effective interventions¡Xhere comes Tai Chi, a centuries-old mind-body practice.10,11
Researchers from Hong Kong, Macau, Europe and America conducted a randomized, assessor-blinded, non-inferiority trial in a single research site in Hong Kong to compare Tai Chi with CBT-I for treating chronic insomnia in adults aged 50 and above. The study enrolled 200 participants, all diagnosed with chronic insomnia under the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) criteria.1
Intervention Details1
Both interventions consisted of 24 one-hour sessions over three months, followed by a 12-month post-intervention follow-up.
Primary Outcome1,12
The primary measure was the Insomnia Severity Index (ISI), assessed at 3 months (post-intervention) and 15 months (12-month follow-up). A non-inferiority margin of 4 points on the ISI was set, representing half of the minimally important difference.
The per protocol analysis showed that at 3 months, CBT-I outperformed Tai Chi:
However, the story changed at 15 months:
This suggests that while CBT-I delivers faster relief, Tai Chi catches up over time, offering comparable long-term benefits. The results of the sensitivity analyses on the primary outcome were consistent with the primary analysis (Figure 1).
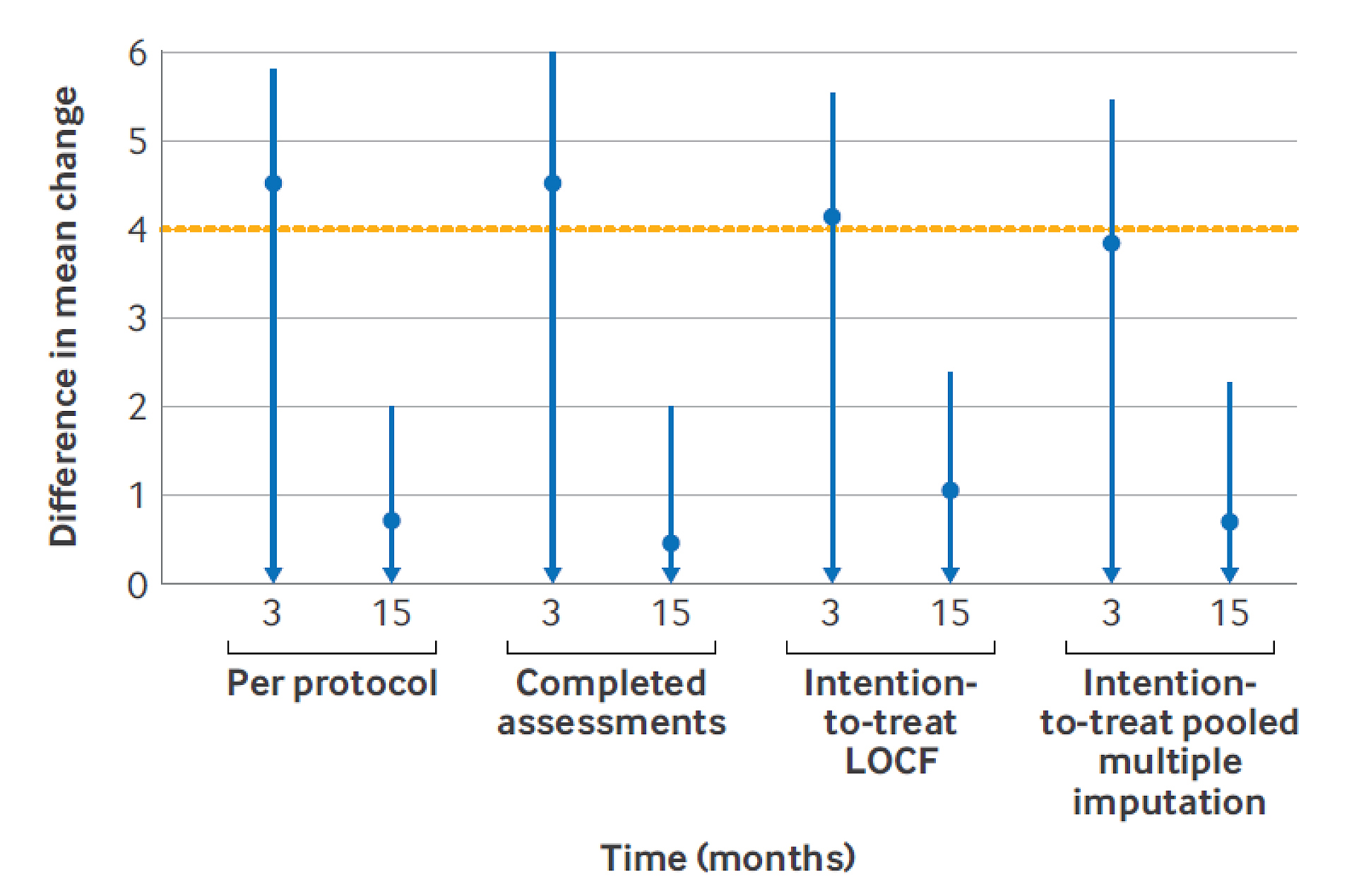
Figure 1: Primary outcome (per protocol analysis): non-inferiority analysis for ISI at 3 and 15 months in Tai Chi and CBT-I groups.1 Sensitivity analyses: completed assessments, intention-to-treat last observation carried forward (LOCF), and intention-to-treat pooled multiple imputation
Secondary Outcomes and Safety Profile1
Tai Chi is more than gentle movement-it's a holistic practice integrating physical, psychological, and emotional components. Research suggests Tai Chi reduces stress, depressive symptoms, and cognitive hyperarousal, all key drivers of insomnia.13,14 In contrast, CBT-I primarily targets dysfunctional sleep-related beliefs, addressing specific maladaptive patterns that sustain insomnia.15
Interestingly, Tai Chi may also influence inflammatory pathways. Previous trials show Tai Chi reduces systemic and cellular inflammation, which is increasingly recognized as a contributor to chronic insomnia.16
The study was conducted in Hong Kong, with 77.5% of participants aged 60 years and older, which may limit generalizability to younger populations or different cultural contexts. Additionally, future studies are warranted to regularly assess adherence to Tai Chi during the post-intervention follow-up period to capture the full tai chi practice behavior.1
Given the high cost and limited reach of CBT-I, Tai Chi emerges as a promising alternative for long-term insomnia management. Its scalability and cultural adaptability make it an attractive option for public health strategies, especially in aging societies.17,18
This landmark trial demonstrates that while Tai Chi may not match CBT-I's rapid efficacy, it achieves comparable long-term outcomes without adverse effects. For millions struggling with chronic insomnia¡Xand for healthcare systems burdened by its costs¡XTai Chi offers a practical, low-cost, and sustainable solution.
References
1. Siu PM, et al. BMJ. 2025;391:e084320. 2. Morin CM, et al. Nat Rev Dis Primers. 2015;1:15026. 3. Wong WS and Fielding R. J Sleep Res. 2011;20(1pt1):117-26. 4. Morin CM and Benca R. Chronic insomnia. Lancet. 2012;379:1129-41. 5. Léger D and Bayon V. Sleep Med Rev. 2010;14:379-89. 6. Edinger JD, et al. J Clin Sleep Med. 2021;17:255-62. 7. Manber R, et al. Sleep. 2023;46:zsac252. 8. Conroy DA and Ebben MR. Behav Neurol. 2015;2015:819402. 9. Baglioni C, et al. J Sleep Res. 2020;29:e12967. 10. Pillai V, et al. Sleep. 2015;38:127-38. 11. Yang G-Y, et al. Complement Ther Med. 2021;60:102748. 12. Morin CM, et al. Sleep 2011;34:601-8. 13. Wayne PM, et al. J Integr Complement Med. 2025;31:499-520. 14. Zou L, et al. J Clin Med. 2018;7:404. 15. Altena E, et al. J Sleep Res. 2023;32:e13860. 16. Irwin MR, et al. Brain Behav Immun. 2024;120:159-66. 17. Siu PM, et al. JAMA Netw Open. 2021;4:e2037199. 18. Wang CC, et al. Am J Public Health 2019;109:755-61.





